Experiencing or being exposed to a traumatic event can be extremely distressing and debilitating. There are times when the effects of trauma can be short-lived allowing us to return to our usual functioning and sense of self.
Other times trauma can be all consuming, changing our mood, behavior, our decision making and our ability to work or maintain healthy relationships and lifestyle habits. The tentacles of trauma can be far reaching, having rippling effects into important areas of our life. Our perception of our self and our relationship with the world in which we live is questioned and our sense of what is safe and dangerous is challenged.
This can lead to a diagnosis of Post-traumatic Stress Disorder (PTSD) or another psychiatric disorder such as anxiety or depression.
“Words can’t accurately convey the anguish the traumatised person experiences…It has an intensity that defies description……”(Peter Levine)
A traumatic event is associated with strong negative emotions and physical reactions.
Examples of traumatic events include motor vehicle accidents, armed hold up, sexual or physical assault, conflicts of war, and an unexpected or violent death of a loved one.
Other traumatic events are more subtle or insidious and include childhood or adult bullying, public ridicule, critical put downs or any other form of emotional abuse. Although these latter events may not be viewed as “traumatic” because there are strong emotional components the brain still registers and treats them as traumatic.
Typical Symptoms Of PTSD Trauma Include
- re-experiencing symptoms including recurring, distressing, and unwanted traumatic memories while awake or in dreams; sudden flashbacks to the traumatic event; reminders or triggers about the trauma causing emotional and physical distress
- avoidance behaviours such as avoiding thoughts, feelings, memories, people, places, activities, objects or situations that remind you of the stressful experience , you may have trouble recalling important parts of the trauma
- negative alterations in cognition and mood such having trouble recalling important parts of the trauma; feeling distant and cut off from other people; having strong negative beliefs about yourself, other people and the world; experiencing fear, horror, blame, guilt, anger and shame; limited or a reduction in positive feelings like love and happiness; increased and harmful behavior or risk taking; or suicidal thoughts
- hyper-arousal symptoms: being “super alert”, watchful, and on guard; feeling jumpy or easily startled; having difficulty concentrating; or trouble falling or staying asleep.
So why are these symptoms present and what happens when someone’s exposed to a traumatic event??
Very simply, when we are exposed to or experience an event that we perceive as traumatic our body does all it can to survive and enacts our fight, flight or freeze response.
Fight, flight, freeze response for SURVIVAL
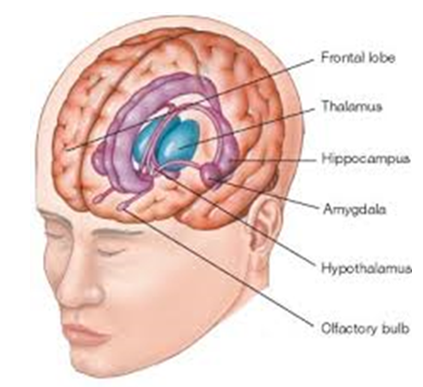
This is an involuntary response which involves the limbic or primitive part of our brain, meaning there is a large emotional and physiological response with lack of rational or higher brain involvement.
We know the fight, flight freeze response is essential for our survival and the release of adrenaline and cortisol is vital and adaptive in acute situations. This is how the brain adjusts to PTSD.
People who are negatively affected by trauma, however, have a sustained and chronic release of cortisol and adrenalin which over time results in neurological and biological changes, including changes to brain structures such as the hippocampus and amygdala that are involved in fear conditioning, working memory, reasoning, planning, problem solving and execution.
Traumatic memories are different to our everyday memories. Everyday memories have the luxury of time to enable the memory to be processed, filed away neatly in our brain’s filing system and then linked up with other processed, adaptive and useful information.
Trapped trauma memories however, do not have time to be processed whilst the trauma is occurring and as a result the trauma memory remains trapped in its unprocessed state, and exists as an isolated memory network with no connections to the other functional and rational information.
The trapped trauma memory remains as a vivid memory and we hold this memory not just in our mind but also our body, hence the memory feels very present and real and as if it is still a current rather than past event. Hence, the trauma cycle continues and the body, mind and self continues to believe danger is present or harm is imminent.
Breaking The Trauma Cycle – Treatment Is Available And Recovery Is Possible
The main treatments for post-traumatic stress disorder include different types of psychotherapy and medication. However, one of the most extensively researched and proven effective treatment for PTSD is trauma-focussed psychotherapy which includes Eye Movement Desensitisation and Reprocessing (EMDR).
EMDR, a relatively new psychotherapy developed in 1987 by Clinical Psychologist Francine Shapiro, is designed to allow a trapped trauma memory to be released, desensitised, reprocessed, and resolved.
On completion of EMDR therapy typically
- The trauma image becomes foggy/less vivid
- There is a removal of emotional charge associated with the trauma and its triggers
- There is reduction of hyper-arousal symptoms
- The trauma memory feels and is perceived as a historical and past event rather than present and vivid
Ultimately, this reduction or cessation in trauma and other related symptoms results in an improvement in our functioning, and our ability to sustain and maintain healthy relationships and employment.
To ensure you are suitable for EMDR, a comprehensive assessment will be completed. Prior to commencing EMDR you will be provided with additional skills and self-soothing techniques to manage and increase your control over your ptsd symptoms.
At the beginning of an EMDR therapy session you will be guided to deliberately bring into conscious awareness and connect with all the components of the trauma memory network including the sensory memory, accompanying emotions, bodily sensations and personal meaning.
Once the traumatic memory is activated your therapist will commence bilateral stimulation (BLS) either through eye movements, palm tapping or thera-tappers.
Although the mechanism is not fully understood BLS produces electrical activity in the brain that enables the traumatic memory to released, changed and be processed.
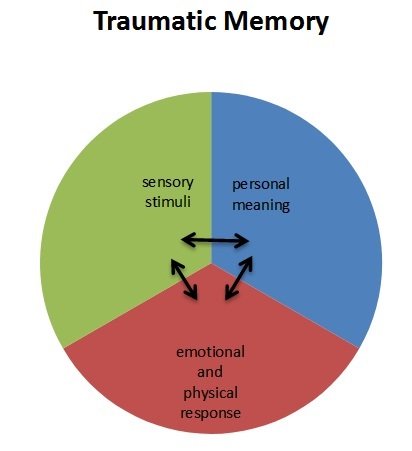 The sensory memory includes details regarding the visual, smell, sound, and touch elements of the trauma memory. The sensory memory is stored in the sensory cortex of the brain.
The sensory memory includes details regarding the visual, smell, sound, and touch elements of the trauma memory. The sensory memory is stored in the sensory cortex of the brain.
The emotional memory is often called the “body memory”, as activation of this part of the trauma memory reactivates the body or physical sensations associated with the event.
The third component, the personal meaning, formed in the prefrontal lobes of the brain, is meaning the traumatic event has or holds for you. It is not the thoughts we had at the time of the trauma, but rather those core beliefs that form afterwards, that are presently held and have emotional resonance.
The aim of EMDR is to process the traumatic memory as quickly and as efficiently as possible whilst maintaining dual attention- this means having one foot in the past (the trauma memory) and one foot in the present (staying connected with present time and not getting ‘lost’ in the trauma memory).
To ensure the processing and momentum is not disrupted your therapist will not engage in lengthy conversation during BLS but rather will keep dialogue to a minimum.
Additionally, your therapist will ask you to “just notice’ or observe the feelings, beliefs, sensations and images that emerge during BLS. It is important during this time not to analyse, sensor or block any of the distressing emotions or bodily sensations that you may be experiencing. Working through the negative aspects of the traumatic memory will clear the way for resolution and recovery.
Your therapist will continue BLS until the intensity and frequency of the negative physical sensations, the emotional charge, and the vividness of the traumatic memory reduces. As every mind and body is different this may take ten minutes, an entire session or several sessions.

The EMDR process is complete when new, realistic and healthy perceptions and perspectives about the self, other people and the world arise and FEEL true.
With EMDR there are no “rights” or “wrongs”, rather an acknowledgement that each EMDR session must be tailored to meet each individual’s needs.
Following An EMDR Session…..
There may be times when you continue to process trauma material for 24-48 hours after an EMDR session. This is your mind’s and body’s way of working towards clearing the traumatic memory. Please make a note of any images, thoughts, feelings, sensations or beliefs that emerge so you can discuss this with your therapist at your next session.
Following your first EMDR session it is recommended to have a friend or family member drive you home, and for all sessions encourage you to avoid alcohol and drugs as this may impede your recovery.
Finally, it is strongly recommended to engage in relaxation exercises and taking some time to prioritise your well-being.
If you have any questions regarding the above please discuss with your medical practitioner or therapist.









That’s a very informative post about PTSD. Many people still don’t know about this illness.
Comments are closed.